42 Year Old Male with a Sudden Decrease in Vision
Case Study: 42 year old male with sudden vision decrease
Dr Robyn Troutbeck
Presentation
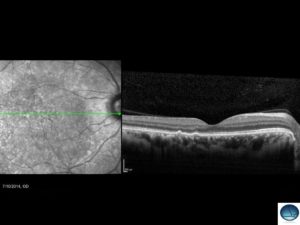
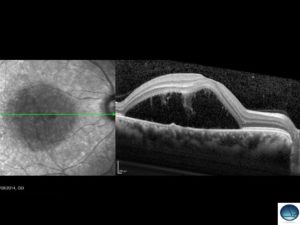
The 42 year old male below presented with a sudden decrease in vision in the RE.
The photo demonstrates significant subretinal fluid over the macular region.
The differential diagnosis includes:
a) Central Serous Chorioretinopathy
b) Vogt- Koyanagi- Harada Syndrome
c) Posterior scleritis
d) All of the above
Click for answer
Answer: d.
More history and examination is required to narrow down the differential. In VKH there is associated granulomatous inflammation in the anterior segment, disc swelling and it is typically bilateral. Posterior scleritis is usually associated with pain. The eye is uninflamed in CSC.
The best investigation to refine the diagnosis is a fluorescein angiogram and it is shown below.
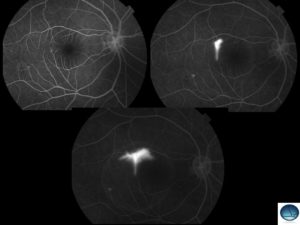
The angiogram shows a classical smoke stack appearance commonly seen in CSC.
What treatment can we offer him?
a) Stop any steroid use
b) Thermal laser
c) Time
d) PDT
e) Anti VEGF
Click for answer
Answer: a, b or c
First ask about any steroid use including creams or lotions and see if these can be stopped given the association with CSC and increased circulating cortisol. This patient was not taking any steroid and had had symptoms for 3 months. Given there is a focal area of leak, thermal laser was used to seal it. Six weeks later the fluid had all resolved.