30 yo female with sudden change in scotoma in L central vision
Case Study: 30 Year Old Female with Sudden Change in Scotoma in L Central Vision
Dr Daniel Chiu 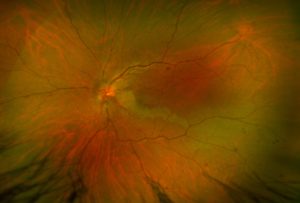
Presentation
30 year old female with sudden change in scotoma in L central vision.
What do you see in the colour photo?
1. microaneurysm
2. vitreous haemorrhage
3. deep retinal haemorrhage
4. papilloedema
5. tortuous retinal veins
6. optic nerve head swelling
7. retinal infarction
A. 1 &4
B. 2, 4 & 7
C. 3, 6 & 7
D. 2 & 6
E. 3 & 5
Click for answer
Answer C.
(The oblique elongated area of prominent retinal pallor running along a retinal arteriole is consistent with retinal infarction in the supplied area of that vessel, rest of the features are self evident)
What is the likely diagnosis?
1. Myopic macular schisis
2. Central retinal vein occlusion with secondary cilioretinal artery occlusion
3. Posterior vitreous detachment
4. Non-specific retinal de-pigmentation
5. Embolic central retinal artery occlusion
6. Raised intracranial pressure with papilloedema
Click for answer
Answer 2.
(This is a pattern sometimes seen in young patient with acute CRVO with very high central retinal venous pressure from an acute occlusion and if there is a cilioretinal artery supplying some of the macula area, the low perfusion arterial pressure in the cilioretinal artery can not overcome the high venous exit pressure and leading to loss of any arterial blood flow and hence an additional arterial occlusion. Not a central retinal artery occlusion. Because it is very acute, much of the classic sign of CRVo may not develop fully yet. In young patient, sometimes the central retinal vein will often re-perfuse very quickly as well)
What would the fundus look like in 3-4 weeks?
1. Florid retinal haemorrhage and oedema
2. Fundus obscuring vitreous haemorrhage
3. Normal appearance with some subtle sclerosed vessels
4. Serous retinal detachment
5. Submacular haemorrhage
Click for answer
Answer 3.
(As explained in answer to Q2)