Quiz Challenge: Elderly Lady with Sudden Vision Loss
Quiz Challenge: Elderly Lady with Sudden Vision Loss
Dr Daniel Chiu
67 yo healthy caucasian woman with one day history of sudden loss of Left vision. Known mildly elevated LDL-cholesterol. Otherwise no hypertension or diabetes
Initial examination shows LVA of CF, IOP 14 at the Eye & Ear Hospital. Noted Left macula slightly pale and much nerve fiber layer haemorrhage around optic disc. Closure venous pressure was elevated.
Subsequent referral to use for further management and seen 2 days later.
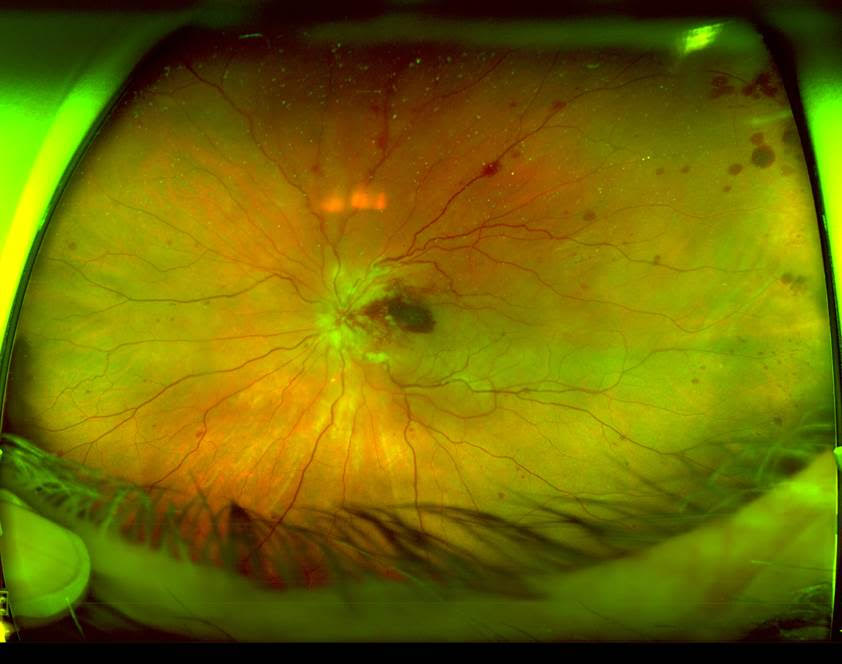
Initial OPTOS Photo in our office. Left vision is HM. Left RAPD present.
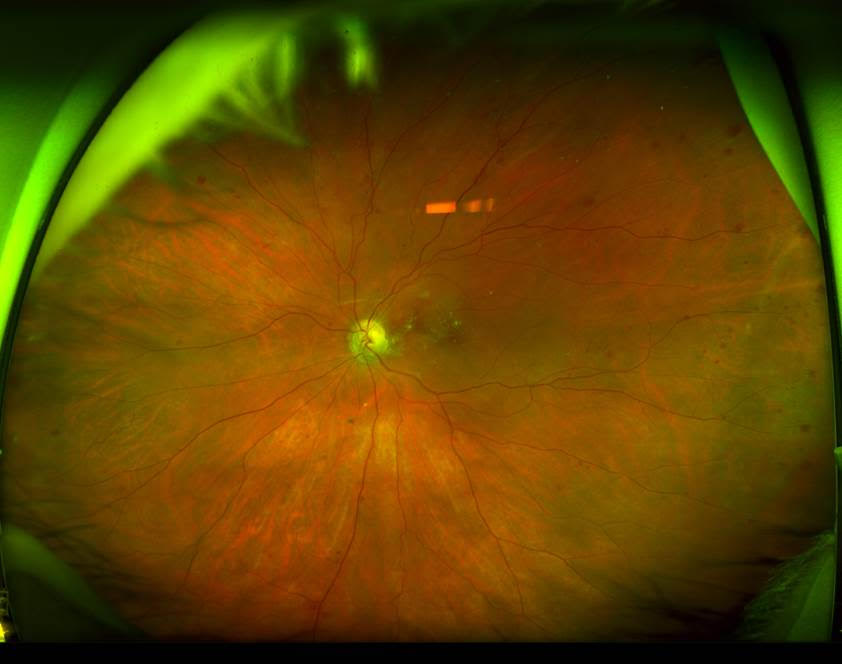
Q1. What is the finding in the Right eye?
A. Choroidal naevus
B. Choroidal metastasis
C. Congenital hypertrophy of RPE
D. Laser treated retinal hole
Click here for answer
D. Laser treated retinal hole
Q2. What is not a key finding in the Left eye (more than one answer)?
A. peripheral retinal nerve fiber layer haemorrhage
B. peripheral deep retinal haemorrhage
C. peripapillary myelinated nerve fiber layer
D. Four quadrant haemorrhage
E. Intraretinal and premacular haemorrhage
Click here for answer
A. peripheral retinal nerve fiber layer haemorrhage
C. peripapillary myelinated nerve fiber layer
OCT shows significant intraretinal macular oedema and some subfoveal fluid
Q3. What is the likely diagnosis?
A. Left central retinal arterial occlusion
B. Left macular branch retinal vein occlusion
C. Left central retinal vein occlusion
D. Left proliferative diabetic retinopathy
E. Left neovascular AMD with fresh macular haemorrhage
Click here for answer
C. Left central retinal vein occlusion
Single dose of anti-VEGF agent was given (Avastin in this case due to poor presenting vision as other agents unfunded)
She was reviewed 4 weeks later.
OCT shows no macular oedema. Some of hemorrhagic changes resolved. Normal retinal venous closing pressure. Left vision still HM.
Photo:

No further antiVEGF given and reviewed 6 weeks later.
OCT again shows no recurrence of macular oedema. Macular map shows some retinal thinning between optic disc and macula centre. Left VA is still HM.
Photo:
Q4. Why is her vision still so poor?
A. Increasing cataract
B. Anterior ischaemic optic neuropathy
C. Submacular scar
D. Macular infarction
Click for answer
D. Macular infarction
Click for summary
This lady presented with a classic picture of central retinal vein occlusion with extremely high central venous closure pressure for a short time. It resulted in secondary cilioretinal artery occlusion. The macula happens to be dominantly supplied by her cilioretinal artery. When the venous occlusion led to a very high venous closing pressure, which can easily be higher than the lower arterial perfusion pressure in a cilioretinal artery, as compared to a higher perfusion pressure of the normal retinal arterial system. In some situation, even a secondary central retinal artery occlusion can happen.
The initial premacular haemorrhage is a result of the venous occlusion, the significant amount of “cotton wool” spots around the disc suggested inner retinal infarction. Subsequent thinning of the retinal in the OCT map especially in the nasal macula is characteristic of cilioretinal territory infarction. Unfortunately, in this case, initial and persistent use of anti-VEGF would have no benefit to her final visual outcome and normal CRVO injection protocol should not be followed blindly.