Inflammation in the Immunosuppressed
Case Study:
Dr Robyn Troutbeck
Presentation
A 54 year old female with a history of rheumatoid arthritis (on methotrexate, prednisolone and tofacitinib) and type 2 diabetes presented with a 5 day history of patchy scotomas, floaters and mild photophobia in right eye.
Clinical findings
- Right Eye was 6/9, IOP 54, 2+ cells in her AC
- Left Eye has 6/6 vision, normal IOP and was quiet.
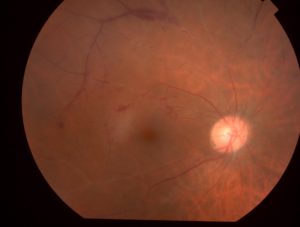
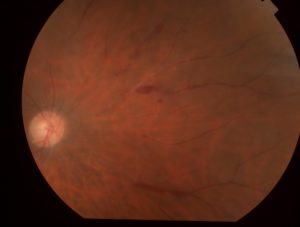
- Posterior pole in the RE is as per attached picture.
What can you see?
There are multiple arteriolar occlusions, some haemorrhage and retinal oedema. Temporally there was a small patch of retinitis, which was difficult to photograph.
What is your differential diagnosis?
Given this patient is immunosuppressed, the first thing to rule out is infection.
The differential diagnosis includes
- acute retinal necrosis
- CMV infection
- toxoplasmosis
What to do next?
A sample was taken from the vitreous and sent for viral and toxo PCR. An injection of foscarnet was given to cover the herpes viruses and she was started on oral valaciclovir and Bactrim.
The tap result was available in 24 hours and was positive for CMV. She had a work up by infectious diseases and her tofacitinib and methotrexate was stopped. She was treated with oral valganciclovir.
Discussion
The mainstay of treatment for CMV in a non HIV patient is to reduce immunosuppression to allow immunreconstition. It is difficult to know how long to treat with the valganciclovir and what to do if her rheumatoid flares. We make sure the retinitis resolves and that she develops no further vascular occlusions before stopping the valganciclovir.
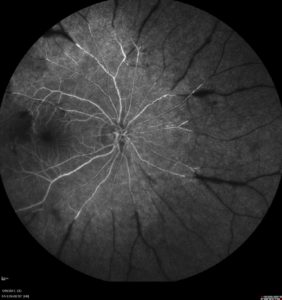
The fluorescein angiogram below shows the devastating effect of this infection with significant retinal ischaemia which will manifest as field loss. In order to prevent neovascularisation she has also had panretinal photocoagulation.